International arrangements to collect and distribute information on epidemic diseases are crucial in times of pandemics, because pathogens ignore borders, political order and economic status. Today states have largely closed their borders in an effort to contain the spread of the coronavirus. But for open societies in a global economy, this can only be a temporary measure. A reliable international tracking and reporting system for epidemic diseases remains crucial because the present pandemic is inherently international. In Southeast Asia, we can build on nearly a century of experience in managing such a system.
The first international system to report and distribute information on epidemic diseases was developed in Asia from 1925, when the League of Nations Health Organisation (LNHO) established its Eastern Bureau in Singapore. The international dimension of epidemic diseases had been put on the League of Nations’ agenda as a result of the disastrous hygienic conditions in large parts of Europe in the wake of World War I. In response to the Spanish Flu pandemic and the severe cholera and typhus fever epidemics in post-war Europe, the League set up a first ‘epidemiological intelligence service’ for the continent. This prompted Japan and Siam to call for a coordinated and permanent engagement of the League in the field of public health in Asia also. After World War II, when the League was reborn as United Nations, the LNHO became the World Health Organisation.
The Singapore Bureau became a regional hub for the collection of epidemiological information, or ‘epidemiological intelligence’, reaching 180 ports as well as ships on sea. Not only did the bureau mark a change in how public health was conceived during colonial times, it was the first organisation with a regional focus in Southeast Asia. During its 17 years of existence until the Japanese occupation of Singapore in 1942, the bureau worked to reduce the prevalence of epidemic diseases in the region and improve the health of colonised and non-colonised peoples of Asia.
While public health in colonial Asia was traditionally aimed at protecting the colonial masters from tropical diseases and ensuring that the indigenous population was able to work, the Singapore Bureau’s establishment was a concerted effort by colonial and independent governments. Through the bureau, the ‘Far East’ was linked to the LNHO and to western innovations in public health and medical science, especially in the field of epidemiology. At the same time, regional coordination on epidemiology in Asia—with independent states, colonies and dominions working together—began to supersede the prevailing focus of protecting the West from diseases originating in the East.
The founding members of the bureau were India, British North Borneo, Ceylon, China, the Federated Malay States, French Indochina, Hong Kong, Japan, Netherlands East Indies, Siam, the Straits Settlements and, as an observer, the Philippines. Setup and operations were funded to a large part by a grant from the Rockefeller Foundation and supplemented by annual members’ contributions. The Singapore Bureau was headed by British, French and Australian directors until it was forced to shut down when Japan invaded Singapore in 1942. Japan, it is worth noting, considered the bureau’s work so important that it continued to cooperate financially and technically even after having left the League of Nations over its invasion of Manchuria in 1933.
The Singapore Bureau began its epidemiological intelligence service in March 1925 by collecting information on epidemic diseases from its member territories and distributing it throughout the region. The bureau established structures to broadcast an epidemiological bulletin free of charge once a week, normally every Friday, via the French wireless broadcasting station at Saigon and the Dutch wireless station in Malabar (Bandung) on Java. The broadcasts were further relayed in North Borneo, India and Madagascar, and were transmitted to the League’s headquarters in Geneva. Some countries and territories also received the weekly bulletins via telegraph or telegram, and more detailed epidemiological information was distributed monthly, quarterly and annually by mail. The bureau’s weekly communications were aimed at members’ public health administrations rather than at a general public, but many of the reports were also published by League of Nations.
The bulletins and reports contained information on cholera, smallpox, plague, meningitis, leprosy, malaria, typhus fever and other diseases. They provided information on everything from quarantine arrangements, administrative and legal public health matters, shipping data, the health of Hajj pilgrims, venereal diseases among sailors to rat infestations. The bulletins were based on a novel reporting system whereby each national administration submitted standardised weekly reports, which, in turn, also had a modernising effect on the participating national public health systems.
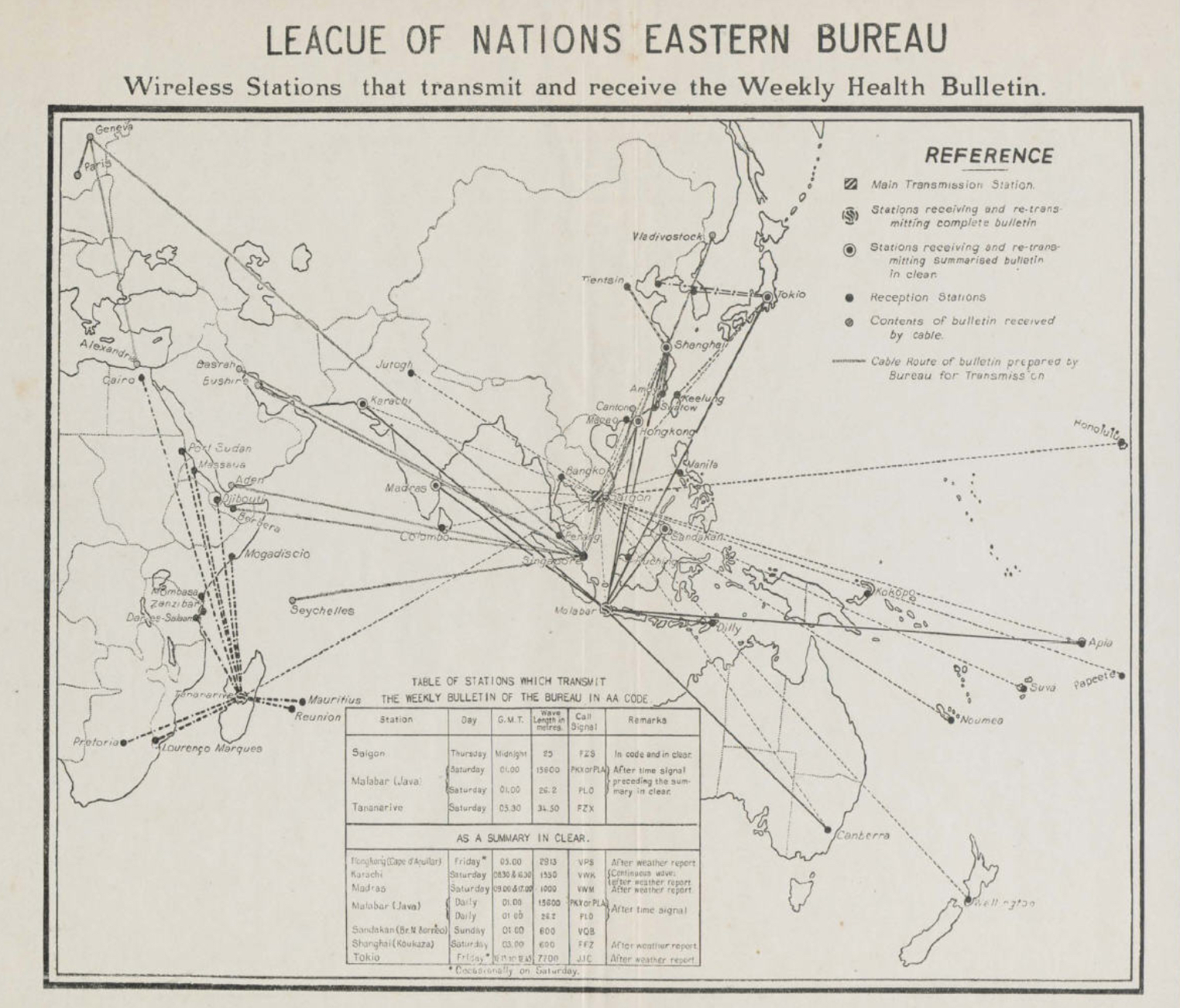
Map showing the wireless and telegraphic network of the Eastern Bureau
The bureau’s reach extended across what was at the time imprecisely called the ‘Far East’: South, East and Southeast Asia, Australia and the Pacific, with connections reaching as far as Eastern Russia in the north, East Africa to the west, and Honolulu in the east. By 1931, after six years of operations, the Singapore Bureau had established contacts with 135 ports in 50 states and territories in Asia, Africa and the Pacific region, up from sixty-six ports in 1926. Later during the 1930s, the bureau reached 180 ports and transmitted its wireless bulletins daily instead of weekly via nine radio stations throughout Asia.
This early warning system allowed port authorities across the region to quarantine arriving ships carrying infectious diseases and reduce the death tolls from recurring outbreaks of infectious diseases in port cities. And by knowing which ships were infected, port authorities also knew which ships were not, thereby limiting unnecessary quarantine restrictions on maritime trade.
Via wireless radio, the bureau was also able to inform ships on sea, allowing crews to avoid calling on ports with epidemic outbreaks or to take precautions if a disease was prevalent on board. In 1932, for example, 188 ships were reported to Singapore as having infectious diseases on board. And in the late 1930s the bureau began including airports in its network, allowing for the disinfection of planes and inoculation or quarantine of commercial airline passengers—procedures we have been reminded of in detail in recent months. This table shows how the bureau tracked ships infected with smallpox and cholera in the year 1936:
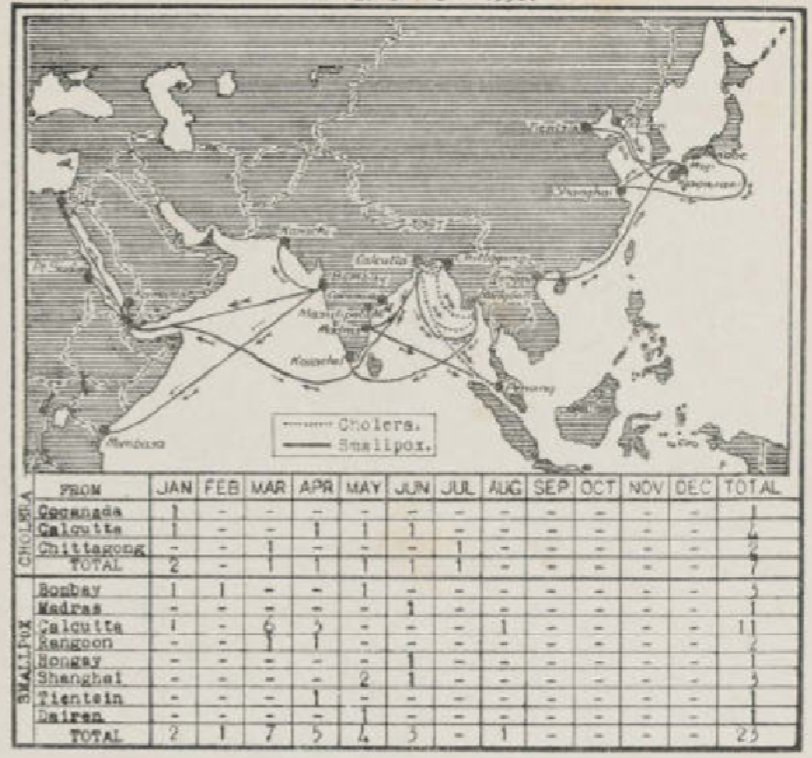
Table and map showing tracked ships with smallpox and cholera infections in 1936
From the field: COVID-19 responses in Central Java
While reports of central government mismanagement are widespread, local and regional officials are implementing sound strategies that account for limited resourcing.
The Kwai Yang arrived in Siamese waters from Hongkong and Swatow, where cholera was spreading, and this had been relayed to Bangkok. Additionally, the crew had reported one death from cholera among the deck passengers while on sea, so the Bangkok port authorities were prepared to isolate the vessel at a quarantine dock. All 466 passengers and crew were examined, 14 suspected cases of cholera were isolated at the infectious diseases hospital and all others remained on board for five days. No further cases of cholera were detected during this period and an outbreak was averted.
This table, drawn up by the bureau in 1937, gives an overview of reported cases of cholera and shows an almost cholera-free region (with the notable exceptions of India and Siam) for the most recent years:
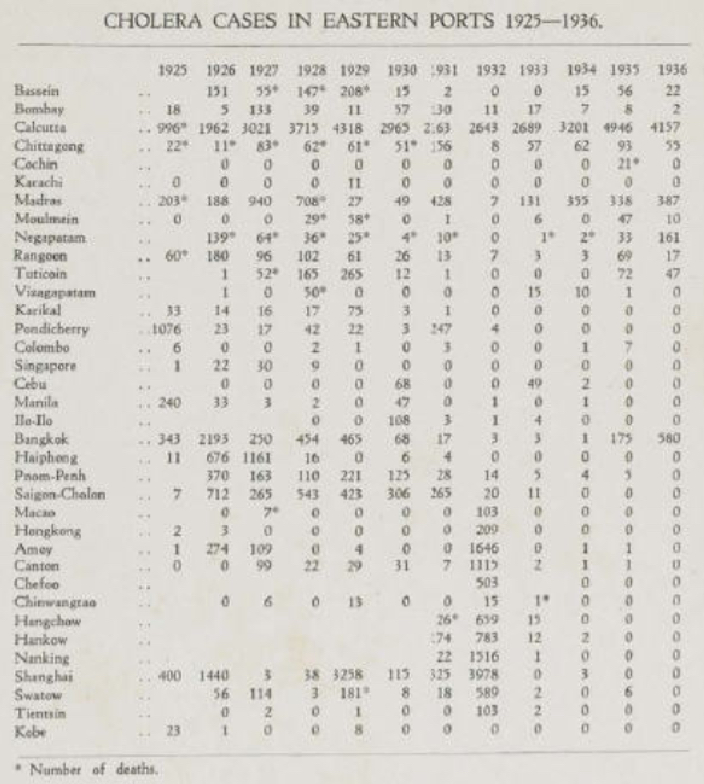
Table showing annual cholera cases across the region
Beyond its work in epidemiological intelligence, the bureau was active in pharmaceutical standardisation, hygiene and port health, training of public health managers and medical practitioners, running annual trainings in malaria prevention, and fostering medical research in a variety of fields. In the eyes of contemporaries, the Singapore Bureau was a real success story. With hindsight, we can say that it indeed marked an important step in improving public health across the region and in the internationalisation of public health generally.
 Facebook
Facebook  Twitter
Twitter  Soundcloud
Soundcloud  Youtube
Youtube  Rss
Rss